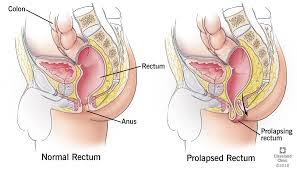
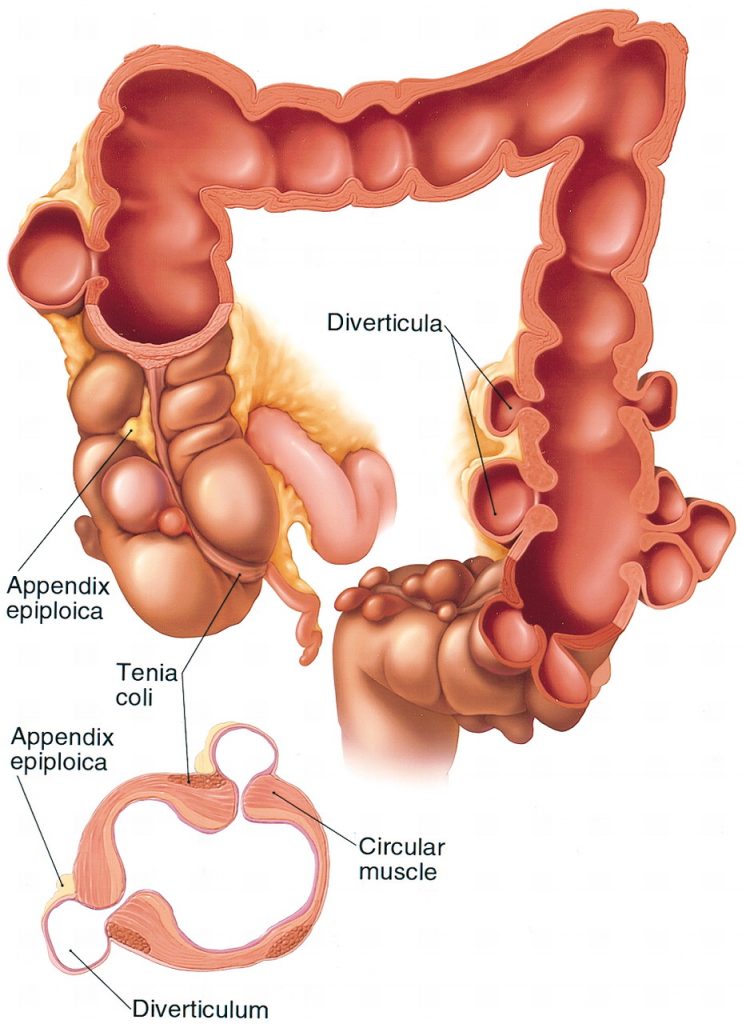
Rectal prolapse is a condition that involves the rectum turning inside out on itself and coming out through the anus. Full-thickness rectal prolapse involves the whole wall of the bowel turning inside out on itself; partial thickness involves the inner lining only.
Symptoms:
The prolapse produces an uncomfortable lump that is red-purple. The lump may spontaneously reduce. The prolapse also causes bleeding with mucus and symptoms of incontinence.
Cause:
There are various anatomical features that may predispose: deep anterior pelvic cul de sac, redundant sigmoid colon, and diastasis of the levator ani. Rectal prolapse occurs mainly in females; the peak incidence is in the 6th to 7th decade.
Investigations:
- Rectal prolapse treatment in Melbourne involves several physical conditions. Bedside examination, including sigmoidoscopy, can diagnose the condition. Examination with the person straining on the commode can diagnose it.
- Colonoscopy: usually performed in the elderly to exclude other problems.
- Examination under anaesthetic may be needed to diagnose the problem.
- Anorectal Physiology and USS: Often used to record sphincter muscle status, especially if incontinence is a major symptom.
Rectal Prolapse Treatment in Melbourne
In children with rectal prolapse, procedures to avoid straining and holding the prolapse back in may cure the problem.
In adults with full-thickness prolapse, surgery is generally required.
Over 100 different operations have been described to treat rectal prolapse.
Transabdominal Procedures:
Rectopexy alone or resection rectopexy, both of which can be done laparoscopically or openly.
Laparoscopic, and now more commonly Robotic ventral rectopexy is a procedure……
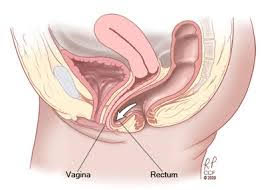
Laparoscopic ventral rectopexy is a procedure now being offered that uses a mesh placed between the rectum and vagina, sutured to these structures, then fixed to pre-sacral tissues. This has a high success rate and is tolerated well in the elderly population. The operation avoids postoperative constipation, which has been a problem in some other surgeries.
Perineal Procedures:
The Delorme procedure, which is a mucosal resection and re-anastomosis, and the Altemeier, or rectosigmoidectomy, are the 2 commonest procedures.Improvement in incontinence can be expected in 50% of cases if the rectal prolapse treatment in Melbourne starts quickly.
Related Links: