Cancer of the colon or rectum occurs when cells lining the bowel replicate in a disordered and destructive manner and these cells also have the ability to spread beyond the bowel into the blood stream or lymphatics to other parts of the body. If you’re considering surgery for colon cancer in Melbourne, understanding these basics is essential.
The sex incidence is about equal and the incidence in our community is 1 in 22. The incidence increases with a strong family history or a recognised genetic disorder (High risk). Colon cancer is one of the commonest internal malignancies affecting humans.
Symptoms:
Before proceeding with surgery for colon cancer in Melbourne, it’s important to recognize the symptoms. Colorectal cancer can be silent until it is large enough to spread into the blood stream or even block the bowel. This is why screening for colon cancer is considered important. Changes in your bowel habits can indicate a problem. This could be unexplained diarrhoea or constipation or indeed a combination of the two. Blood noticed within the bowel motion or in the toilet can mean a problem. Abdominal pain or lumps can mean a problem. Anaemia (low blood count) due to slow bleeding from a bowel tumour can cause tiredness and puffed-out symptoms. Many other symptoms can happen if a bowel cancer spreads from its original site.
*Please note: These symptoms can be from many other conditions and don’t necessarily mean you have bowel cancer.
Comprehensive Investigations Before Surgery for Colon Cancer in Melbourne
- Beside Exam: Bedside examination including rectal “glove” examination and sigmoidoscopy should be done.
- Colonoscopy: This examination gives an inside view of your colon allowing biopsy(snippet) of any abnormal looking sites. The examination is performed in registered centres or hospitals and requires bowel preparation, a period of fasting and a sedative aneasthetic.
- Barium Enema: This is an X-ray alternative to colonoscopy which shows an outline of the bowel lining due to dye and air being inserted. Biopsies can’t be taken.
- Virtual Colonoscopy: This is a Scan that new model CT scanners can perform. Bowel preparation and insertion of air are currently required. Biopsies cannot be taken.
- CT Scan: This is performed to give information about the area outside or next to the bowel tumour and also distant to the tumour.
- MRI Scan: This is a special scan generally reserved to get more focussed information of the thickness of rectal cancer.
- Rectal Ultrasound: This is an ultrasound probe used to stage the thickness of rectal cancer.
- PET Scan: This scan is reserved for special reasons and gives information on your whole body.
- Screening: Screening tests are tools used to identify a group in a normal risk population that may be at higher risk of having disease present at the time of the test.
- Faecal Occult Blood Test (FOBT): This tests for any hidden blood in your stool and if present means you have a higher risk of bowel cancer being present. Large trails have confirmed this test to be useful and when used appropriately can uncover people with bowel cancer at an earlier stage.
- Colonoscopy: This is a tool generally used for diagnosis, but when used for screening, it is more accurate than any other test.
Recommendations:
The American Society of Gastroenterologists have recommended faecal occult blood testing and regular sigmoidoscopy in people with normal risk at age over 50. When considering surgery for colon cancer in Melbourne, these screening recommendations should be taken seriously. The Australian government through its health authorities are gearing up for population based screening with FOBT in the near future.
Treatment:
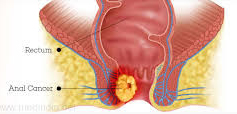
Surgery with excision of the cancer has been the cornerstone of treatment in cancer of the colon and rectum for cure. In some cases of rectal cancer radiotherapy has been used for cure. In anal cancer combination radiotherapy and chemotherapy has been the cornerstone of curative treatment.
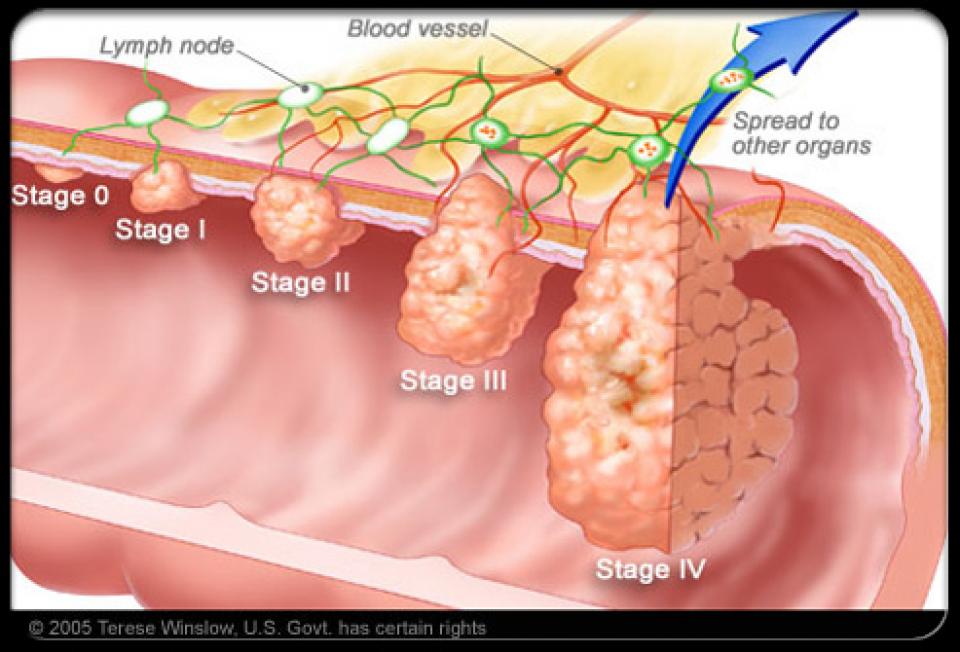
Stageing of Bowel Cancer
Patients with bowel cancer are staged after pathological examination of the resected section of bowel after surgery, and sometimes an attempt is made to stage bowel cancer before surgery by means of ultrasound, CT scan, MRI or PET examinations.
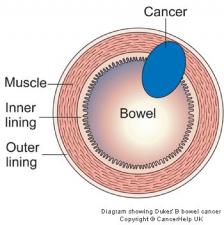
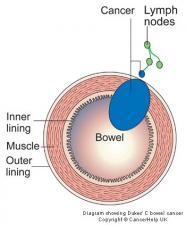
Bowel cancer has traditionally been staged by a method called “Dukes” stageing named after a famous pathologist called Cuthbert Dukes. For simplicity sake this stageing method will be presented, although there are other stageing systems.
*Please note: every effort is made to minimise risk, but colon surgery places relatively high stresses on your body during its recovery and healing phase. Assessment of individual risk for surgery is difficult and figures quoted in consultation are averages.
The Principles of Surgery Are
Stage A: bowel cancer confined to bowel wall
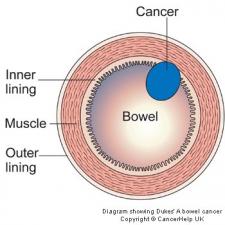
Stage B: bowel cancer penetrated through the bowel wall.
Stage C: bowel cancer involving spread to lymph nodes draining the bowel segment.
Stage D: bowel cancer involving spread to liver.
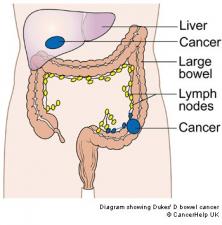
The stage of bowel cancer has a bearing on the treatment offered and also the prognosis(the chance of cure in the long term).
The principles of surgery are:
For patients undergoing surgery for colon cancer in Melbourne, the main principles include, clear removal of cancer and draining tissues, with a view to joining the bowel ends together if possible. Minimising risk and maximising function post-surgery. Surgery is usually performed in medium-large hospitals. Surgery can be performed in the open or laparoscopic technique, although for those with bowel cancer laparoscopic (key-hole) surgery is reserved for small tumours in parts of the colon that are easily accessible. Bowel preparation, blood tests, ECG(cardiograph), Chest X-Ray are all performed routinely as part of your anaesthetic work-up. Your hospital stay is 7-10 days but can be less for key-hole surgery.
*Please note: every effort is made to minimise risk, but colon surgery places relatively high stresses on your body during its recovery and healing phase. Assessment of individual risk for surgery is difficult and figures quoted in consultation are averages.
“Adjuvant” treatment:
Treatment involving radiotherapy and chemotherapy before or after surgery is done in consultation with oncology and radiotherapy physicians. Common courses of radiotherapy are 6-8 weeks long. Common courses of chemotherapy are 6 months long. Agents used in chemotherapy are constantly being refined, and each have their own side-effect profile. Please discuss with your oncologist. Radiotherapy has both short and long term side-effects, please discuss these with your radiotherapy physician.
Follow up:
After surgery for colon cancer in Melbourne, follow up is generally performed to try and detect any recurrence of tumour as early as possible. Regular office visits for examination and blood tests are usual especially in the first 3 years after surgery. Repeat colonoscopy is generally organized every 2 years for the next 6 years after surgery.
Related Links: